Being a mom in the age of the internet can be overwhelmingly scary.
Google “prolapsed pelvic organ” and you’re surrounded by terrifying images and horror stories on mommy forums that leave you with more questions and less hope.
Navigating life as a mom is hard enough. You don’t need your Google search results to scare you to tears.
Yes. Having a prolapse can leave you feeling worried and less than confident. But it doesn’t have to be so scary. Your life isn’t over. Your running/lifting/enjoying all the things life doesn’t have to end.
There are some key strategies and tools you can use to feel strong and confident again.
And the first step to feeling more empowered is to know exactly what you’re dealing with. The second step is knowing how to manage your symptoms and enjoy your life without constantly worrying if something you do (or don’t do) will make it worse.
What Exactly Is Pelvic Organ Prolapse (POP)?
In the bottom of your pelvis are your pelvic floor muscles and tissues. They act like a hammock or a trampoline supporting your pelvic organs (like your bladder, uterus and rectum).

A prolapse happens when these muscles and tissues get damaged or become incredibly weak and can’t properly support one or more of your pelvic organs. Once that support is compromised the organs fall down farther in the pelvis than they’re supposed to sit.
There are a few different issues and events that can cause prolapse. Like a long, hard pushing phase during labour, use of instruments during labour (forceps or vacuum), the drop in estrogen during menopause that can weaken pelvic floor tissues, and chronic lung diseases (like asthma) that cause you to cough a ton, to name a few.
Whatever caused your prolapse, it’s important to know that this is not your fault. It isn’t. You have enough guilt in your life, you don’t need to add “I did (or didn’t) do something and now I have a prolapse” to the list.
The best thing you can do is get help as early as possible. You want the best chance of getting as much function back to the muscles and tissues as possible. But it’s never too late and there are plenty of options to help your pelvic organs out – regardless how long ago you had your baby.
There are a few different types of prolapses.
The 3 most common prolapses are:
- Bladder (Cystocele)
- Uterus (Uterine)
- Rectum (Rectocele)
If you have one of these types, it simply means that your bladder, uterus, or rectum is drooping down instead of staying perched up where it’s meant to be.
It’s also possible to have more than one prolapsed organ. Both your bladder and uterus could be prolapsed, for example.
There are also different grades or classifications of prolapse:
You can read more about the specific classifications right here.
For now, here’s the basic outline:
- Grade 0 (no prolapse)
- Grade 1 (the organ or organs are slightly drooping down, while still being more than 1 cm above the level of the hymen)
- Grade 2 (the organ or organs have come down a bit further and are 1 cm or less above the level of the hymen)
- Grade 3 (the organ or organs have slid pretty far down and are now more than 1 cm below the level of the hymen)
- Grade 4 (the organ is causing your vaginal wall to bulge out of your vaginal opening)
With every sentence I type (Grade 4, I’m looking at you) I feel compelled to write “It’s okay! Please don’t stress! There’s hope!”
I know this can feel overwhelming and the opposite of fun, but stick with me. No matter how mild or severe your symptoms are, there’s absolutely hope. There always is.
And the truth is that symptoms vary and no two cases are the same.
Some women have a grade 3 or 4 prolapse with very little to no symptoms.
Others have a grade 1 or 2 prolapse with significant symptoms.
This is why it’s important that you focus less on the classification and more on your unique symptoms.
And remember that regardless what’s going on for you, there are options and strategies that can help.
Signs You Could Have It
It’s estimated that around 50% of women have some degree of prolapse after giving birth. But only 10-20% of women report symptoms of prolapse.
This means that most women with prolapse don’t actually have symptoms. It’s not severe and as long as they take steps to support their core and pelvic floor recovery postpartum – which I recommend all women do – they likely will continue to be asymptomatic throughout their life.
The truth is that our pelvic organs don’t need to stay in the exact same place our entire lives. They’ll likely shift during pregnancies and postpartum, throughout our menstrual cycle, and during menopause.
This is normal.
The key is to simply be aware and be mindful about any symptoms you may have without obsessing over them (which can be easier said than done if you’re Googling all the things worrying that you have prolapse and wondering how to fix it).
And take the appropriate steps to ease your symptoms if they do come up.
If you do have symptoms, they may look something like this:
- Heavy feeling in your vagina
- Feeling like you need to pee but it won’t all come out
- Lump or bulge in your vagina or vaginal opening
- Feeling like something is falling down or dropping when you cough, sneeze or jump
- When you sit it feels like you’re sitting on something – like a small ball or an egg
- Issues with leaking
- Having problems pooping (constipation) or feeling like you can’t fully empty your bowels
- Painful sex
- Not feeling much, or having less sensation when you do have sex
- Back pain that gets better when you lie down
- Abdominal pain
- Having trouble keeping a tampon in
- Getting bladder infections a lot
Remember – you can get all or just some of these symptoms.
Can You (Safely) Exercise With POP?
Yes. You can exercise with POP.
You’re not destined to a life without fitness. We just need to make sure that you’ve got a handle on supportive strategies (like proper core engagement and breath) and the fitness things you’re doing aren’t making your symptoms creep up.
So what exactly is safe exercise for POP?
The answer is, it depends. (Which is not the answer you were hoping for, I know. But hang in there. 😉).
What kinds of exercises do you want to do?
What kind of breathing + engagement strategies are you using?
Do your symptoms get worse? Better? No change?
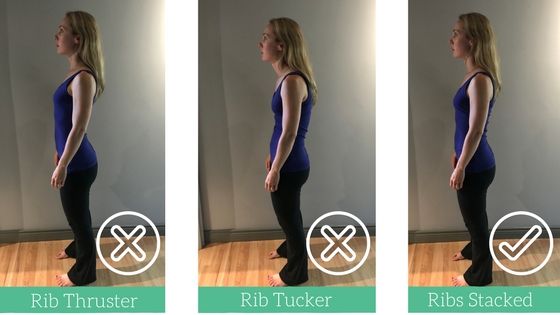
How does your alignment look?
There are so many factors to consider and there isn’t a one-size-fits-all-moms approach to exercising with prolapse.
Unfortunately, the medical prescription most commonly given to women with prolapse is that they shouldn’t lift more than 5lbs. 5lbs?! Most newborn babies weigh more than 5lbs! So that is not even close to realistic for any mom.
And that’s the worst thing to hear when, pre-baby you loved heavy weight lifting, running, or just a more high intensity, high impact kind of workout.
But remember, having POP doesn’t mean you can never lift heavy, join the rec. soccer team, or do more high intensity, high impact exercises ever again.
We just need to pay close attention to how your body responds and ensure your breath, alignment and technique are spot-on so that you’re getting stronger and getting little-to-no symptoms.
You’d be surprised how a simple tweak here and there can make a huge difference.
There are plenty of ladies – like prenatal and postnatal fitness pro Haley Shevener – who have POP and enjoy an athletic level of fitness.
It simply depends on what you’re doing, how you’re doing it, and how your body is responding.
Bottom line: you can exercise with POP.
The key is to be mindful of your strategies (like form, breath, and alignment), choose exercises that are right for your body, pay attention to your symptoms during and after exercise, and work with pros who know how to train a woman with POP so you can get back to doing what you love.
So How Bad Is It? Really?
There can be a lot of fear and confusion and overwhelm around the idea of a prolapse. Most of that stems from the fact that hardly anyone talks honestly about it in a practical way (beyond “Don’t lift heavy weights”), and the internet is full of horror stories.
The truth is that prolapse is scary when you don’t completely understand what you’re dealing with and you don’t know how to “fix” things.
You might feel less confident about having sex, or doing certain exercises, or getting pregnant with another baby because you’re afraid it’ll make things worse.
But there are pros and tools and strategies you can use to help get your life back.
Here’s what I recommend you do:
Step 1: Book an appointment with a pelvic health physio
This is a critical first step because a pelvic floor physiotherapist or physical therapist can do an internal assessment to see what exactly is going on in there and give you the next best steps for your body.
No two cases of POP are the same so we want you to get what you specifically need.
You can find a pro in your area using the links on this page.
Curious what exactly will happen during your appointment? It’s not as scary as it sounds. The lovely ladies at Bellies Inc. put together this great video to give you the low down on what will likely happen during your down low assessment:
Some pros will also get you to stand up, and maybe even do some gentle exercises, and do an assessment while you’re standing or doing certain movements. I think this is a fantastic idea because sometimes when we’re laying down it’s hard to tell exactly what’s going on. But once we’re standing and moving, it’s easier to get the whole picture.
Remember – you are in charge of your own health so find a great, qualified pro to help you out.
If you aren’t happy with the experience you’re getting, find someone else.
This is your body. Your life. You don’t have to just live with the discomfort and worry. Find someone who supports your goals and is willing to do whatever they can to help make that happen.
Step 2: Pay attention to what exercises and events bring on symptoms
Does running make you feel heaviness in your vagina?
If you’re on your feet all day do you feel like you can’t control your bladder by 7pm?
When you do that deadlift with that weight does it feel like something is bulging out of your vagina?
Do your symptoms get worse when you’re ovulating or menstruating?
When you’re tired or stressed, do your symptoms creep up more?
Paying attention to what’s going on in your body as you go about your day and your workout is crucial to better understanding the steps you can take to help feel stronger.
It may simply be a matter of trying different exercises, different variations of an exercise, doing less reps, taking more rest, or starting out with less weight and then progressively challenging your body in a way that makes it feel like it can handle the pressure.
It may also help to adjust your training around your cycle (which can be helpful for all women – not just women with prolapse). If you know that you get more symptomatic when you’re ovulating, that can help inform the type of exercise you do during that period.
And of course you’ll also want to work on your breathing techniques, getting in better alignment, and engaging your core in a way that supports your pelvic organs (instead of generating more downward pressure into your pelvic floor).
You don’t have to stop doing the exercises you love forever.
But if you’re getting symptoms when you do that particular exercise, with that particular weight, in that particular way, we need to troubleshoot and figure out what’s going on so we can get you to a place where your symptoms are no longer an issue every time you try to workout.
Step 3: Release & relax and also build up your pelvic floor strength
It’s pretty obvious that if your pelvic floor is compromised, working on strengthening it will likely help alleviate some (and maybe even all) of your symptoms.
But what you may be surprised to hear is that releasing and relaxing your pelvic floor is key too.
In fact, many women discover that a tight pelvic floor is actually creating more symptoms for them. Yes. A too tight pelvic floor can actually make your prolapse symptoms worse.
This can be especially true if you’re under a lot of stress. When we’re stressed, we have a tendency to tense up. Think of how tight your shoulders can get after a hard week with a teething baby and work deadlines galore!
Now imagine what your pelvic floor is doing. Right?
That’s why doing some pelvic floor-specific relaxation and meditation exercises can be really effective.
You can do a mobility flow like the video below to help release the tension, and you can also spend 2 minutes in meditation using a progressive relaxation technique.
For progressive relaxation, lay down on the floor, close your eyes, and take a deep breath in, then exhale as you tighten your pelvic floor muscles (do a kegel), then inhale and release and relax all the muscles in your pelvic floor and your bum.
Do this 3 – 5 times.
These techniques can be especially helpful when you’re getting more symptoms than usual.
We also want to focus on strengthening your pelvic floor.
This doesn’t necessarily mean that 5 sets of 10 kegels daily are what you need. It may be the case. But not always.
Rehab can look like kegels and clamshells. Or it may be squats and rows. It really depends.
And the truth is that, there really isn’t a set of “prolapse healing” exercises that you can do because it’s not just about what exercises you do, it’s also about how you do them.
So (at the risk of sounding like the world’s most broken record) pay attention to your breathing, your alignment and your technique. And be curious about how your body feels during and after a certain workout or exercise.
Check in with your postpartum fitness pro, physio, midwife, or doctor to see what the best options are for you.
And if you are exercising – especially in those early months of playing around with exercising with prolapse – remember to exhale and engage your core and pelvic floor as you do the hardest part of the exercise. I call this the BED Mantra. It can help your pelvic floor better support your organs during your workout.
Step 4: Explore the idea of a pessary
If you want to run, lift heavy, jump rope, and generally be more active but you’re worried those things can (or already are) making your prolapse symptoms worse, or you simply want some relief from the symptoms you’re getting in your daily life, you can look into getting a pessary.
A pessary is a small silicone device that can be made in many shapes and sizes. You put it in your vagina as a space occupier or to help support your pelvic organs.
You can think of it like a sports bra for your pelvic organs.
Don’t worry, you won’t even be able to feel a properly fitted pessary.
For some women a pessary not only helps them feel physically able to do the workouts they want to be doing, it also helps them relax mentally. Having the extra support can help them ditch some worries about making things worse.
So if you find yourself clenching your vagina (consciously or unconsciously) during your workouts (or all day, every day) because you’re worried about making your prolapse worse, a pessary could be your new bestie.
If you’re curious, this is something you can chat about with your physical therapist, physiotherapist, or doctor.
The best news? A study of 106 women with stage 2 or greater POP showed that most women saw a significant improvement in POP symptoms when they used a pessary.
So a pessary can work incredibly well if you find the right choice for you.
Quick tip: I have heard some doctors say that young moms don’t need pessaries. That they’re only for older ladies. This is absolutely untrue. Why wait when you can improve your quality of life now?
So if you get some pushback, find a healthcare provider who is more supportive of what you’re going through and the options that can help.
And remember that it may take a bit of effort to get the right fit. Some research shows that, “On average, 2 to 3 fittings were required until the appropriate pessary was found.”
So if it’s not fitting right, don’t be afraid to go back and get re-fitted. You deserve to feel good and this means getting a pessary that fits well.
What if I’ve done all that and my symptoms are still really bad?
If you’ve worked with a pro to rehab your pelvic floor, your alignment, engagement, and breathing strategies are on-point, you’re getting some relaxation and release sessions in, and you’ve tried a pessary, but you’re still getting symptoms and you feel like you need something else to help, then surgery may be a great option for you.
This is something you’d want to consult with a urogynecologist or other pro about (different pros may take on this role depending on where you live).
Just remember that surgery is typically best for women who have already tried rehabbing their pelvic floor and have tried other strategies and options so that the chances of a successful surgery is improved.
You can think of the pelvic floor rehab as prep-work for surgery because you’ll know how to properly support your pelvic organs post-surgery and boost your chances of having the results you’re wishing for.
Surgery is an option. It just doesn’t have to be the only option and usually isn’t the first step you’d take.
The bottom line is that it’s your body, your choice. Do what feels best for you.
There’s Always Hope
Growing and birthing tiny humans is not an easy task.
Add to that the potential for issues like prolapse and you can end up feeling depressed, alone and wondering if you’ll ever feel like yourself again.
But it doesn’t have to be that way.
I hope that this post gave you some tools and strategies you feel confident running with (maybe even literally!) Because there’s always hope.
Prolapse can be a scary, overwhelming, “I have so many questions” thing. But it doesn’t have to be. You now have a better idea of who to turn to for support and the tools you need to feel stronger and more confident.
Use ’em.
There’s no such thing as 10 Quick Steps to Healing Prolapse but you don’t need them.
Take the right small actions every day and you will see progress. It may be slow. It may look more like an up and down squiggle and less like a straight line. But it will still be progress.
You’ve got this.
You deserve this.
💜 Jenna
P.S. Know of other moms who are dealing with prolapse? Send them this post and remind them that there’s always hope.
I’m still left confused with what “progress” looks like. Feeling uneasy even working out may plague some women and be the be-all-end-all issue to fix, but what about those of us who work out only moderately? It those of us not concerned with being able to work out? I hardly have time to eat and shower with a full time job and a 4 month old. I’m willing to do some kegels, but I’m not up at the gym or out running miles.
My version of progress would be my grade one cystocele and rectocele going away, going back inside and out of sight, being fully healed and whole and normal again. This article really focused on working out, as if it were the main concern. Maybe it is for some, but is there any hope that it could heal and go away? I’ve seen 5 doctors about it, and received responses that range from “no, it will only get worse with age,” to “at 1 year postpartum, you’ll be fully healed.” I have no idea what to expect and I’m really short on hope.
Hey there,
I hear you. It’s incredibly frustrating when you can’t get a definitive answer and you’re worried that things won’t get better. But please don’t lose hope. There are plenty of women out there (active and not) with prolapse who live very normal lives. It is doable.
The thing is, there are so many factors that go into this that it’s impossible for me to say with absolute certainty that XYZ will happen for you. I know that’s frustrating and not what you want to hear at all. You want a straight answer. You want to know that if you do _____ you’ll heal and be back to normal.
The problem is that every body is different and every situation is different so I unfortunately can’t say exactly what will happen for you with total certainty.
That doesn’t mean that you should be afraid or uneasy to workout or do anything active because you’re worried that you’ll make things worse. If you’re interested in exercise – not necessarily high intensity stuff but the more moderate stuff you mentioned – I highly recommend you check out Haley Shevener – you can find her on Instagram and she also has a prolapse Facebook group. She’s incredibly active (and lifts some heavy kettlebells! 🙂 ) and she has prolapse. I think she would be a great person to bring back some hope into your life.
And remember – you don’t have to want to get back into intense workouts for the strategies I mentioned in the post to work for you. They’re for anyone – regardless what kind of exercise (if any) you want to get back into.
So…
Have you been to a pelvic floor physio or physical therapist?
Have you started to do some core and pelvic floor rehab exercises – beyond kegels (squats, mini band lateral walks, bridges, hip thrusts…)?
Have you been working on your alignment (butt untucked, ribs stacked over hips)?
Have you been focusing on your breathing and how you engage your core and floor when you pick up baby, etc?
These are all key things to work on, even if you don’t plan on going to the gym regularly.
Another thing to consider is that, if you’re breastfeeding, you still have some hormones circulating that could be making your soft tissues more flexible and “looser”. A few months after your baby weans you may see some more positive change as the hormones leave your system and your body settles back into a new normal. This may be what some drs are referring to when they say “It’ll heal in one year” they may be referring to the hormones in your body right now.
There are not guarantees that it’ll heal completely but I have met plenty of women who focus on the steps I mentioned above and they (thankfully) have been able to get their life back and feel strong and “normal” again.
I really hope this has given you some ideas of where to go next and ultimately given you some hope. You have so much stress in your life and your baby is so young that there is plenty of time to get it all worked out. Take your time. Focus on one step at a time and you’ll likely see that progress you’re hoping for. Let me know if you have any follow-up questions 🙂
Jenna please listen to your Dr. This is not something to mess with. If minor that is one thing but if it is really affecting your life you may need help. I am not even over weight and I have prolapse yet people say exercise, lose weight bla bla bla. It is not true. It might be for very few women but others no.
Thanks for this! I’m 5 weeks postpartum and, while I’m not sure I have prolapse yet, all signs point to some prolapse issue. (Feels like something is stuck in my vagina, there seems to be bulging tissue not far from my vaginal opening, I’m having constipation issues, etc.) My first postpartum OBGYN appointment is next week. Luckily, I know a great pelvic floor physical therapist and I already have appointments booked with her next month, and my symptoms seem to improve when I do kegels (the way the physical therapist taught me, with proper release after tightening) and when I avoid certain triggers (bending up and down to do laundry while wearing my baby).
This is the only heartening thing I found while consulting Dr. Google. Everything else seemed to indicate I’d never feel normal again (and possibly never have sex or run again) if it were a prolapse issue. I just needed something to make me feel better until I could see the experts, and this article did that. So, thanks!
I’m so glad you’re on top of this, Meg and have a great PF PT to help you out. You definitely sound like a smart cookie and what you’re doing now will go a long way to get you back into all the exercise, running and sex you can handle 😉
Keep in mind that it’s still really early as well and your body may still be working on some spontaneous healing so focusing on having great alignment as much as possible, breathing/engaging well, and not overdoing it physically can be really helpful to support that process. You’re absolutely doing the right thing by paying attention to your triggers and adjusting your strategy or avoiding that thing altogether when you feel symptoms creep up.
I’m sure your PT will have some more goodness and hope to share with you. I know Dr. Google can be vicious and tear-inducing at times so I’m glad you found this post helpful and hopeful. That was my goal and I’m so grateful it gave you the pick-me-up you needed.
And just an extra FYI – I’ve actually heard from several women that sex actually makes their prolapse symptoms lessen/feel less intense. Maybe it’s the orgasm? Who knows! So definitely don’t worry about not having sex again – that sounds awful. There are lots of options in that regard!
Keep your chin up and keep going until you find the experts/pros you need to support you in reaching the goals you have. You may not be able to “go back” but you can feel strong and awesome going forward with the right tools and support.
This is a really lovely collection of information on prolapse. As some in Pelvic Floor Therapy for a hypertonic pelvic floor, recently pregnant, and terrified of a prolapse….this really helped put my mind at ease. Thank you!
I’m so glad it was helpful, Jess. I know there’s a lot of scary information out there. Just remember that every woman is unique and just because one woman’s story turned out a certain way does not mean yours automatically will too.
Congratulations on your pregnancy! I hope there’s more joy than fear going forward 🙂
I just found out I have 2 prolapses. And yes while it might not sound so bad for some it is bad for others. It is affecting my kidneys. So at this point it is not good. My grandma has prolapse. Her bladder falls all the time and has to be put back if not she suffers so much pains she can not stand. My aunt had a triple prolapse and hers was extremely bad as well. You might want to talk about how not bad prolapse is but don’t give one side of it give everyone the whole box of truth.
Hey Kristy, it’s really awful that you and other women in your family are suffering with so many negatives that can come along with prolapse. It was not my intention to make light of it – it can definitely be serious for some women – and I absolutely don’t suggest that prolapse is no big deal or something you don’t have to worry about at all. My intention was to provide some support, answer some questions and give some hope and options to women who feel like their life is over and they don’t know how to get the help they need or they’re wondering what next steps they could take. I didn’t want to focus on the doom and gloom – rather I wanted to avoid cultivating more fear and opt for more hope and resources to help instead.
Have you or your grandma and aunt been able to see a pelvic health physiotherapist? I think you all could benefit from working with someone who could help – and perhaps even look at the potential of a pessary or even surgery if that’s the best option. I hope you find the support you need 🙂
I so agree. Anyone who can say this isn’t so bad I’d like some of what they are smoking. This has ruined my life. I wouldn’t wish this hell on my worst enemy. It’s on your mind every second you are in your feet. Unfortunately can’t go thru life laying down. Some days I just cry and wish for it to end
Me to. I am so depressed and humiliated. I hate that Im incapable of doing anything without behaving like a 80 yr old woman. Im so sick of reading how its not so bad….just change everything you do and you’ll be fine posts! Wear a plastic thing for the rest of your life. Let numerous random strangers poke you and judge you consistently. Dont jump, dont squat, dont lift anything over the weight of a kettle. Watch everything you eat. Push it out of the way when you poo. Brace every time you sneeze or cough..forever.
I feel like women are not advised of these risks properly AT ALL, it should be one of the main topics in all gynaecology consults for pregnancy and in general. I would never have had a Natural birth if it was properly discussed BEFORE the fact. The way gynaecologists categorise our anatomy after birth, mine feel into HER normal range so she didn’t tell me!!! 12 years later and it is to late for any changes.
I feel my world
has crumbled. In a huge silent lonely mess. I am absolutely devastated and cry everyday alone.
Me too . I feel disgusting and like im a flabby,loose, shot out old hasbeen. I’m afraid my husband is gonna leave me for someone younger and tighter than me. I have 9 kids and still want one more but my obgyn didn’t recommend it. It makes me so sad. I feel like my vagina is gonna fall out completely and I’m gonna be useless . I already feel broken. And struggle often with insecurity and depression. I don’t know how to drive and my anxiety keeps me on edge. It’s so hard to get to appointments and I don’t trust my current obgyn. So I’m helpless and I just feel like my life will never be normal or feel happy again. I wish all the lady’s on hear love and happiness in your lifes and hope you are all able to get your lifes and body’s back to the way you want them. Much love and God bless always. Sabrina C.
Hey SD,
I hear you. I remember feeling very frustrated and worried when I was experiencing pelvic floor issues and heaviness after the birth of my second child. It’s awful and no one should have to go through it. I in no way want to minimize the pain and emotional + mental stress that having a prolapse can cause.
My intention with this post was to give hope and options so women who are struggling know that they are not alone and that – especially if they aren’t getting the care they deserve from one provider – they seek alternative options until they find a solution that works for them.
I want you to know that it’s never too late. Women who had children 20+ years ago can see positive changes with the right support. And the truth is that women who have had C-sections, and even men can actually get prolapse too. So having a vaginal birth isn’t the only cause of prolapse.
But regardless how it happens, regardless how long ago it happened, there are options and I hope you find the right approach that works for you ❤️
You are so right. I wish I had an elective c section( which reduces the risk to a minimum) every day of my life now. I Start to cry when i Think about how great my life would have been if i wouldnt have had a natural birth. Everything is like it was before birth. That is what all the midwives and friends and my Mother told me.. weil not for me
It’s awful that you’re experiencing this, Zu. I hope you find the support you deserve ❤️
Hi fellow females w/ lovely “girl-organ-issues”!! I’m 45 & pre-meno. My 1st baby (25 yrs. ago)was vaginal & my last 2 (HUGE!! 12 lbs. & 10 lbs.) were c-sections. The 10 pounder is almost 15 yrs. old now & I literally just had my very first pokey-outie surprise 10 minutes ago & Googled about why my partners in crime think they can just go wherever they want all of a sudden!!!! Looks like I’ll be calling a Doc. & praying that my husband & I don’t feel like there’s a (loose) stranger in our bed!!!! GOOD LUCK TO US ALL!!!!!
Me too, not sure how much more I can take. I have cried daily for the past 2 years, was suicidal snd am on such an array of anti depressants now . It has absolutely ruined my life. I’ve had the surgeries, done the pelvic floor and am still incontinent and have constipation. Trying daily to accept this way of existing
I feel like I have some type of prolapse but not sure where to go or who to talk to. It affects my everyday life and I can barely make it thru my 8 hr work shift because I stand on a line all day. I have never had kids so people act like I can’t have any kind of prolapse but i know what I feel
That’s an awful experience to go through, Kim. Especially trying to convince people to believe you. Do you have the ability to see a pelvic health physical therapist or physiotherapist? Has your doctor or OB given you an actual internal pelvic exam? Those are two places I would start.
I hope you get the support you deserve!
Hi Jenna, this post really brought light into my life. I recently went through my fist birth, a beautiful big baby, who unfortunately had passed away late in the pregnancy. On top of that I wasn’t cathetered in time, which probably might be one of the causes for the uncomfortable bulge I’m feeling now when walking or standing. Running has been my go-to for dealing with anxiety, and the idea of never being able to run again has made my sorrow intensely worse. This gives me hope that there can still be some joy in life, thank you!
Hey Stef,
I just want to reach through the computer and give you the biggest hug! I’m so sad that you’re going through this – I hope you have a ton of support helping you right now. And I’m also proud of you for recognizing that there’s hope and that you’re trying to find a solution to help get back into running. You definitely deserve that joy back in your life so please don’t give up.
I’m grateful for your kind words and that this post gave you some hope. That is exactly why I wrote it. Please don’t hesitate to reach out if you have any questions or anything. I’m here for you. Big, big hugs!
Hi. I’m 61 and got my prolapse 3 years ago. I have a pessary and it’s helped somewhat. I have to work full time and take care of all the housework and animal Care. I feel some days like i just want to die. I cry all the time. The symptoms are ALWAYS there. Heaviness pain pessary makes you discharge constantly so yucky wet uncomfortable all the time. I have to live for my family and pets they love me and can’t survive without my income. Honestly I have had many health issues but this has ruined my life
I am honestly looking for the “right” thing to say to help feel supportive for you Cathy, but I know there’s nothing I can say that would make you feel the way I wish you could feel. It is so awful that you have to go through this and you feel so much pain, sadness and hopelessness. Have you talked to your family doctor about getting a referral to a psychologist or counsellor who could help support you? Have you tried seeing a different physical therapist or physiotherapist to get some different options/another approach to see if your pain can be minimized some more? Because you’re experiencing so much intense pain and it’s impacting your entire life, have you looked at the option of a surgical intervention or something other than the current pessary you have to see if your quality of life could be improved more? There are tons of options and I know it may feel like there’s nothing you can do but so many women are able to have a great quality of life – even after getting a pretty grim diagnosis – with the right tools and support. I hope you can find the support you deserve!
This is how I feel I have been to 2 different emergency rooms and a gyno bc I have been experiencing problems and nobody believes me bc I don’t have any kids. I have never thought about suicide so much in my life until now. I feel ur pain
Your comment is extremely troubling to me, Kim. Suicide is serious and I’m very concerned for you. Please do not give up.
You can have prolapse without having kids – men can get prolapse. So my recommendation is that you find another gyno who will give you an actual internal pelvic exam – a proper one – to get to the bottom of whatever is going on.
Another option is to look for a pelvic health physical therapist. They can also diagnose you and are educated in this area.
Again, please do not give up. There’s hope and we’re here supporting you! ❤️
You are so interesting! I don’t think I’ve read a single thing like that before.
So good to find somebody with unique thoughts on this
issue. Seriously.. thanks for starting this up. This website is
something that’s needed on the internet, someone with
a bit of originality!
Thank you! Glad you enjoyed it 🙂
I have been suffering with a prolapse for almost 7 years now. tried the pessary and it hurt so much and also had trouble getting it out. the horrific bulge is always there now and it repulses me so much. Tried the kegel, still am, but not helping much. This has definitely hindered my life. I finally decided on surgery but not until the spring because I don’t want to be having a hard time with inclement weather on top of it. I have a very good and kind dr. but am really terrified since I have always suffered with severe anxiety. I live alone and wonder how I will be able to get through it. I’ve opted for a vaginal procedure that closes up the area with stiches. it is considered the easiest, quickest recovery time. still, i’m sooo scared but cant live like this. Has anyone had any kind of surgery and was it as horrible and incapacitating as it sounds? Greatful for any reply. ggm
Hey Gloria,
That’s awful that you had such a negative experience with the pessary 🙁 Were you able to try different sizes/shapes or have a different provider try to fit you for one that could work better? I know it’s not always easy finding the right fit but I hope you were given some options.
Something that could be incredibly helpful for you to look into for before and after surgery is working with a pelvic floor physical therapist. Even though you’re getting the surgery they can still help you strengthen your pelvic floor to help boost the chances of a successful/positive surgery experience and help with your post-surgery recovery. There is sooo much more to strengthening the pelvic floor than kegels and they could help you explore some options.
Also – have you looked into hiring a nurse or caretaker to come help you at home? If your finances allow for it that could be a helpful option for support post-surgery (and help lessen your anxiety over the whole situation).
I hope the surgery is successful and yes – if anyone has any advice or experience to share with Gloria, please do!
I just found out I have a prolapsed bladder yesterday. Since I got home from my appointment I have been reading and researching non stop. I’ve collected several links to refer back to and read many testimonies. Right now the doctor prescribed an estrogen hormone cream and I have not read that here from anyone. I will be using it for a month. I have read about pessaries – never heard of them until yesterday – and that might be something that will help me. But what I found interesting was this lady who said she uses a super tampon wrapped in a condom to avoid dryness and it has helped her. Another lady said she uses a menstrual sponge that expands to keep everything in place. Mind you I’m only sharing things I’ve read but it – along with this site – has given me some hope too. I had a partial hysterectomy years ago and the GYN doc said I never had to have a pap. Bad advice. Had I gone for periodic check ups I would have been able to prevent this from happening along with hormone replacement therapy when I went through menopause. My heart goes out to all the young mothers here. But like you said there is hope. I hope this helps someone as I continue to look for more ways to be encouraged.
Thank you for sharing your story, Oanneh! It can be so helpful and encouraging to know you’re not alone when other women share similar experiences. I hope you find a long-term solution that works well for you. Pessaries can absolutely be a fantastic option!
I just had prolapse surgery for cystocele rectocele and had my uterus removed. The rectocele portion of the surgery has been the worst. I don’t want to scare you from surgery but the recovery is much harder than I thought it would be. I am 5 days out and can finally move around a bit. I did have an added complication. I also had to have someone come in for the first 3 days to help with meals etc.
Thank you for sharing your experience, Susan. I hope your recovery is continuing to get better and better!
Gloria, not sure if you’ll see this as I can’t see a date of when you posted but my aunt has just gone through the op to stitch her vagina after suffering prolapse of uterus and bladder. Took her 6wks to recover (total rest) but she is feeling happy with her decision. She was in her 70s. Hope that helps.
Hi, I guess I’m not you’re average reader as I just turned 57:) yesterday . I’ve had 7 pregnancies w/6 children born. The youngest is 24 now. About 2 years ago I felt my first bulge and was clueless. After much googling and research I was horrified lol Since then I’ve been to see a GYN who said it was actually mild. However it’s an annoying feeling to be sure so Tuesday I’m going to see her again to get fitted with a pessary. I really hope it works well for me. Your article was so encouraging and helpful and clear! I’m going to share it with my daughters! Thank you so much!!
I’m so glad you’ve found the support you deserve, Susan! It’s so common for women to start developing symptoms during menopause – when our hormones change we can end up with less support in our pelvic floor.
Definitely check in with a pelvic floor physical therapist if you have that option – they can help you strengthen your pelvic floor so that you can hopefully get even more support and relief with some customized exercises + the pessary. And remember that the pessary should be comfortable. It should fit well so you don’t even remember you’re wearing it. So go back if that’s not the case. I hope all goes well! 🙂 And thank you so much for sharing!
I would also fall under “not the average reader” category as I just turned 23. I have never had sex, so it goes without saying that I have never had a child. I have all the symptoms of the last stage prolapse. At first I thought it was a cyst, but no. It prolapses every time I get my period (for the past 3 or so), and it has gotten worse this time. It is very uncomfortable to me even walk or sit. I want to have children in the future and want to live a normal life. I’m so nervous and scared and have no idea what to do
Hey Rosa,
It’s awful that you’re experiencing this!
My first piece of advice would be to see your doctor, OBGYN, or pelvic health physical therapist/physiotherapist. They can give you a diagnosis and next best steps based on your particular situation. Have you had a chance to do this?
Hi Jenna, thank you for this post, it gives me hope and I really need it. When you say “work with pros who know how to train a woman with POP” who do you mean?
You’re so welcome, Elizabeth. I’m so glad it’s giving you hope ❤️ What I mean is that – if you’d like to workout (which I recommend you do to help build strength and stability to help support your core and pelvic floor) – you’ll want to find a personal trainer or fitness pro who’s familiar with prolapse and knows how to help you rebuild strength, feel confident in the gym, and help you learn how to truly listen to your body and be mindful of any symptoms that are coming up that suggest you need to change something up (modify a movement, stop doing something, try a different breath or engagement strategy, that kind of thing).
Having the right pro help you navigate through this can be so incredibly helpful. I’m obviously available to help support you and I have other trainers I know who could be a great fit as well (shoot me an email if you’d like to chat more about potentially working with me or you’d like help finding someone else – jenna@jennadalton.com).
Remember, you can absolutely have an active life with POP. You just need the right approach.
Thank you so very much! Your words were just what I needed and a push for me to address this and find a PT. Please know your words can and are changing lives for the better ❤️
Thank you so much for your lovely comment, Danielle! I hope you can find the support you deserve. Shoot me an email if you’re having trouble finding a PT and I’ll see if my network has someone they can recommend ❤️
hi, am 26 and jux discovered am suffering from prolapse.i want to know if i can get pregnant in future?
Hey Abigail, you can absolutely get pregnant again. If you have access to a pelvic floor physical therapist that would be a great place to start to get tips and strategies to help you feel supported throughout your pregnancy. Many women with prolapse go on to have future pregnancies and recover well postpartum. It’s absolutely possible and a future pregnancy won’t automatically make your prolapse worse. 🙂
I’m 62 and just diagnosed with anterior prolapse (bladder). Never had kids so had no knowledge of pelvic floor issues. Its ridiculous that women are not informed of how to keep this area healthy nor that menopause and lack of estrogen can cause issues. As well as feeling sick and depressed about this (makes me feel useless, old and that my life will never be the same) I am also angry that there is no awareness being publicised. We older women are led to believe incontinence (my first symptom) was old age. It isn’t. Had I gone to the dr straight away I probably could have avoided the prolapse. As it is I am now awaiting to see a urogynaecologist and a womens physio but I am so sad to be dealing with a possible lifelong issue.
It’s horrible you’re having to deal with this, Jaki. And you’re so very right – it’s awful that more education around women’s bodies, pelvic health, and hormonal changes throughout the lifespan and the impact it can have is not more commonplace. Women deserve better. I hope that you have a great support system in place to help you navigate this.
Hi Jenna
Your information has been the clearest and most encouraging I have read to date!
61 years old and not suffering with a cystocele grade 4 I feel sorry that this is now a health issue in my life. I have seen a pelvic floor physio and she has been very helpful. I feel depressed that my activities like dancing, gardening, lifting and gym work all has to be curtailed. However I am somewhat encouraged by your advice and hope life will get better and may well try a pessary in the future?
I read the young mum stories and feel somewhat luckier that it has happened to me post menopause and not when my babies came! Here’s to positivity and grasping another challenge in life.
Hey Mary,
I’m so glad that this post was clear and encouraging for you! I know it can be depressing when you feel like you can’t do the activities you used to love right now. But I really believe that you don’t have to give up hope. There are so many options for you.
It sounds like a pessary could be a wonderful topic to bring up with your physio – she could potentially help you get fitted for one or refer you to someone who can.
I love that you’re staying positive and I know that with the right support you’ll be dancing up a storm again 🙂
Mary I’m 61 too … trying to feel positive … post menopause is certainly a challenge and I’m thinking a pessary May be helpful too . Thankyou for sharing and from one 61 year old to another I’m wishing you all the best and to the younger mums in here please don’t give up find the couple things that are helpful and rest up
I’m absolutely terrified. I’m 39, never had kids and am not sexually active at the moment. I am also quite overweight 🙁
I’ve noticed my symptoms becoming worse over the last 6 months. Not every time, but sometimes I find it very hard to empty my bladder. I go, and 5 mins later I need to go again. I often need to push into my vagina, or against the skin near my vagina to empty my bladder. I can also feel a hard bulge falling into my vagina. When running or skipping I often feel the need to urinate. When I sneeze I often leak.
I don’t have any bowl issues.
I don’t know what to do. I live in a small town in Australia, and have limited access to specialist doctors. I’m so scared that it’s going to get worse!
Hey Kodi,
It’s awful that you’re going through this and that you’re terrified – I get that there are so many fears and unknowns in this and it can feel really scary.
Have you talked to your doctor about this? That would be the first step because it may be prolapse or it may be something else. So instead of going down the rabbit hole of Googling every night and losing sleep over this, if you haven’t yet, book an appointment with your doctor and get a check-up.
Another option – that’s available right now – a lot of pelvic floor physiotherapists are doing virtual sessions since the pandemic has caused them to shut down their clinics. There’s no physical examination (you won’t have to get naked on camera!) but they’ll talk with you, get to understand your symptoms more, and help you figure out a plan.
You can search for Australian (or global) PTs using this link >> https://jennadalton.com/find-a-pro-in-your-area/
Please find some help, Kodi. I know that this is scary, but it will feel so much less scary when you have a team of people helping you find some solutions. You don’t have to live like this forever. If you can’t find a PT in your area or that’s not an option, let me know and we’ll look at other possibilities ❤️
I’m 41 and a breast cancer survivor. I was diagnosed with rectocele (which I think has been going on ever since I have birth 7 years ago), and am scheduled to see a pelvic floor therapist next week. Really worried though because sometimes it’s near impossible to defecate without some pushing (and splinting), but yesterday that caused vaginal pressure all day long, and it happened again this morning. I worry this will never get better and I am doomed to get surgery that might not even help that much.
I know it can be really scary thinking about all the possibilities, G. But you’ve taken the first step. You’ve booked an appointment – which is amazing – and hopefully the pelvic health physio will be helpful, supportive and give you more hope.
In the meantime, I highly recommend you get off Google 🙂 I can tell it’s only increasing your anxiety and making this whole situation feel even worse. Yes it could be what you fear, yes it’s scary to think about that possibility. But you may not need surgery, you may have an amazing physio who helps you feel great, you may find answers and support and the tools you need.
I hope your appointment goes great and I hope you get the support you need and deserve.
Hello, I am a 78 yr old woman who has had priblems for many many years. It never stopped me from doing the things I wanted to do. Bur, recently it has gotten much worse. It is a 4 plus! Whenever I am standing or walking the prolapse is making it impossible! To add to this, I am the caregiver for my husband who had a stroke! I have to help him stand and must di many things that make it worse! I am trying to figure out what to do! I was told twenty yrs ago to have a hysterectomy!confused right now!
Hello Marilyn,
First I want to say your husband is lucky to have you to support him, and it must be very challenging at times being that support system for him.
It sounds like based on your comment that you’ve seen a pelvic health physical therapist or your doctor and had a diagnosis of a grade 4 prolapse, correct? Did they give you options for next steps?
Typically when it’s quite severe (like a grade 4) surgery is considered one of the best options. Have you talked about this with your physical therapist or doctor? Have they given you some options to think about? If I were in your shoes that would be my next step – talk to my physical therapist or doctor and weigh the options. Because you don’t have to just live with this. I hope you get the care you need and deserve!
Thank you for this post. I just found out today that I have a prolapse. I have a follow up appointment with gyno/uruologist on December 30th. I feel more informed about questions to ask and strategies to try. The part that is the hardest for me is I literally can’t stop thinking about it. Just that unusual feeling is driving me crazy. Any thoughts on what I can do to support that area until my appointment? I knew I had a relaxed pelvic floor since having my daughter 14 years ago but then the other day I forced urine out because I was in a hurry and I felt a sharp pain. Ever since then something feels different. I saw a midwife RN today and she said she can see my bladder so she referred me to gyno/urologist. She assured me she has seen much worse but it still terrifies me. Once again……really appreciate your informative post. I’m not alone.
You are absolutely not alone, Kerry. And it’s important you remember that this is not your fault. It’s so common for us to assume that if we’d only done this, or not done that, that we wouldn’t be in the position we’re in. But that’s just not true and I hope you aren’t beating yourself up about this.
I remember when I was about 6 weeks postpartum with my second I got a bad cold that ended in a bad cough. I kept feeling heaviness in my pelvic floor and I was worried what it meant. I couldn’t stop thinking about it. It drove me bananas! And then one day I decided that I would do what I can to feel strong and comfortable again but that I’d stop obsessing over it.
It wasn’t easy to just “let it go”, but now – after going to physiotherapy, following my postpartum strength training program, and being mindful of my form and technique and breathing and all that good stuff – I feel great.
There are always options – regardless how bad it may seem. And while it won’t be easy to put it completely out of your mind, every time you think about it you could try saying to yourself something like, “It’s okay, I’m taking steps to take care of this. The best thing I can do right now is relax.” (Especially since a tight pelvic floor or constantly clenching can actually contribute to prolapse too so we don’t want to clench with the assumption that it’ll make it better. It won’t).
I found walking and meditation really helpful to get my mind off things. And I also just kept reminding myself that, regardless what happened, I could be happy. It wasn’t always easy, I had to consciously make that choice every day, but I’m so glad I did. Good luck with your appointment and please keep me updated. I’d love to hear about your progress ❤️
Thank you so much for posting something positive about this. It gives me some hope. I love your attitude and am definitely trying to stop thinking …if i only would have…I could have avoided this. Idk why there is so much shame and self blame with this condition it sucks. Ive been devistated since getting diagnosed with stage 2 cystocele. Im only 30, have 2 kiddos to carry, love working out, and have a career that regularly requires me to lift people. I regret not demanding c section for both my 9 lb big headed babies. My Dr insisted vaginal birth was what I should do, but of course never mentioned this could happen. This sensation of prolapse is the worst thing I’ve ever experienced and the most afraid Ive ever been that my life will never be the same and only get worse. Im only 3 months postpartum from my 2nd and about to start PT and see a urogyn. Will ask about pessary too. Cant stand the constant pressure pain and feeling like organs falling out at all times. Its driving me crazy lol . Also just went back to work can the lifting make it worse or would a pessary prevent?
Is there any chance this prolapse can reverse or become asymptomatic? How much PT until you got relief / max potential results? Do you know many people that did surgery and had positive results ?
I’m glad that this post is giving you hope, Aj!
It’s hard to stop thinking about it, isn’t it? It’s like me saying, “Don’t think of a pink elephant!!” Of course all you’re going to think of is a pink elephant 😉
The truth is many of us have natural tendencies to blame and self-shame over all things motherhood, and this area is no different, unfortunately! Which is why I want to advocate for women to get more than just physical support for prolapse. Mental health is an important area to hone in on too because conditions like this, with the symptoms, the anxiety, the guilt and shame, it can take its toll and make it even harder to cope.
And I hear you. After my second baby I had a lot of pressure-like feelings in my pelvic floor and anxiety over it getting worse or not getting better. I hated the heavy feeling and just wanted it to end!
While I would love to give you answers to your questions, the truth is that I can’t give you definite solutions and suggestions without knowing your exact symptoms, checking in with your PT to see what they recommend, and all that good stuff. So my suggestion to you is to bring all the questions you have to your PT. Don’t hold back. I’m sure they’d be happy to answer all your questions (and if they aren’t, find someone who will!)
Pessaries and surgery can be extremely helpful for some women. Working on rebuilding strength and lifting and breathing in ways that support your pelvic floor and core can also be very helpful.
I have seen and heard from so many women who are now asymptomatic that I always have hope. It’s not an easy road but it’s a very worthwhile road. I hope this gives you hope and I hope you have the support you need from your PT!
Thank you for the informative article! I admit that after almost 4 years of dealing with a cystocele which is grade 3 and a rectocele, probably grade 2 that I have learned a lot. I am also able to state I am glad I did not discover them until age 61. For years my gynos would say, oh your bladder has dropped. Not once did anyone ever mention the word prolapse! They, of course attributed the drop to my two births. When I finally discovered and understood what had happened I was horrified and suffered a terrible depression and anger. It was as if the docs felt, hey, no big deal. Had I known this at a younger age I’d have driven myself nuts with worry. I eventually decided on a ring pessary with support. What a psychological and physical life saver to me. So far it is still doing its supportive job. I am able to insert and remove it myself. Of course I am careful as to the precautions mentioned regarding exercise, lifting, etc. l am unable to consider surgery so who knows what the future will hold. I will soon visit my urologist as I suspect I may be adding a urethrocele to my collection. Believe me, I still get depressed at times but my pessary has been a good friend to get through.
I’m so glad you’re having a positive experience with your pessary, Nancy. It sounds like you got a great fit.
It really can impact your mental and physical health, can’t it? It must have been awful discovering that you had no idea this was happening with your body. While it may have been scary to be told this had happened, I’m glad you have the support you need now. Thank goodness we’ve come a long way in support for postpartum women!
And keep in mind that you can still be active despite having prolapse. Thousands of women enjoy an active life with little-to-no symptoms when they have the right tools, support and cues. It doesn’t have to limit you – especially now that you have a pessary to help 🙂
Hi, thanks for the helpful info! I’m only 17, and I’m 90% sure I have a prolapse I have a doctors appointment booked for next week, so I’ll find out then. But I have a large bulge and I think it’s a uterus prolapse, about stage 1.
Everyone I’ve heard of having this is fairly old or has children , so it makes me feel sad. I would say I’m very healthy and in shape and work out a lot, so I just don’t know why this has happened to me. I hope it doesn’t get worse and worse 🙁
Hey Flora,
I’m so glad you have a doctor’s appointment booked. Another great option would be getting in to see a pelvic floor physical therapist or physiotherapist.
I imagine that things feel pretty scary, stressful and uncertain right now. While I can’t promise any magical fixes, I can remind you that thousands of women live amazing, fulfilling, fitness-full lives with prolapse. It does not have to get worse and there are so many options to support you (and your pelvic organs!)
I hope the appointment gives you the support you need ❤️
Thank you so much! If it really doesn’t get any worse then that should be great, because it doesn’t bother me yet, other than harder to put tampons in. But that was really reassuring to here, thanks. I guess it can happen at any age? Also I have been trying to learn kegal exercises to try to prevent or even reverse the symptoms. I will also ask my mum about pelvic floor physical therapy. Thanks so much for your comment xx
Yes, it can absolutely happen at any age, Flora. And men can experience prolapse too – not just women.
I do highly recommend seeing a pelvic floor physical therapist. They’ll be able to give you an accurate diagnosis and give you exercises and such to help you feel better and more confident in your body. You are not alone and there are so many options to help you through this!
I thought I would let you know that apparently I don’t have a prolapse but just a low uterus. Which is reassuring. Also the internet can be a weird place and make people think they have problems when they don’t. Maybe others thought this. But you were really helpful throughout
I’m so glad that you found that out, Flora. And you don’t have prolapse. That’s great news! I’m sure that was a scary experience for you.
And you’re right – the internet can be weird and awful, but thankfully there are also great supportive people ready to help. Glad you got the answers you needed!
I’m 54 years old with a stage 2 bladder prolapse. I’ve had 4 previous operations first when I was 35 I had a vaginal hysterectomy, within a year I had another operation where mesh was inserted and attached to my pelvis as I was still suffering with a prolapse. When I was 43 I underwent a vaginal repair as prolapse was back. I haemorrhaged 2 weeks post op and ended up needing an emergency operation and blood transfusion. I have within the last 5 years experienced a further prolapse and now have stage 2 cystocele prolapse. I’ve had intense physiotherapy and lost weight but still the prolapse constantly bothers me and hinders my activities. I am under a consultant be he is wishing to postpone a further operation until I am older. I have tried pessaries, one fell out,, the other was very painful and had to be removed. I feel i have a constant heaviness in my vagina, pain increases on movement, particularly bending and sitting for long periods. I don’t have an active sex life as prolapse makes it very uncomfortable. I’m waiting to speak with the consultant again but not sure what he can suggest. I have a lot of scar tissue from previous operations. A further operation will involve shortening my vagina and will prevent sexual intercourse. I feel very low in mood. I am currently inserting pessaries twice weekly into my vagina releasing estrogen. I was on HRT for years but have been off them a year now. Any advice would be appreciated. I have read some really inspirational stories on here and I now know I am not alone. Thank you for listening to me. I live in Bristol UK.
Anne,
My goodness you have been through a lot! Your willingness to stay as positive as possible amongst all this and see the stories on here as hope really warms my heart. You are a trooper!
One common thread I have heard from several women experiencing prolapse is that they have had to go through several physiotherapists, or other professionals before finding the right fit. Remember that you do not have to settle if you’re not getting the support you want and need. I understand there are limitations that may stand in your way – healthcare, finances, location, etc. However, if at all possible, book appointments with other professionals in your area. Look at other options.
Luckily, in the time of COVID right now, we actually have an opportunity to explore telehealth options and seek support from professionals we may not have otherwise been able to see since they are not local to us. So look outside your hometown to see what else is available within the UK.
There are always options, always other opinions, always hope. Keep moving forward. As hard as it is to keep pressing on at times, you deserve treatment that leaves you feeling supported (physically and mentally!) I hope you find the support you deserve!
I’m 34 and have a bladder prolapse I went to see a specialist and i have to say I left her office with more questions and uncertainty for the future because she didn’t tell what my diagnosis was nor did she discuss anything with me but she did give me a referral for pelvic rehabilitation I was feeling depressed and alone and I stumbled upon this blog and I don’t feel so alone now because I know there’s other women going through the same thing and I’m thinking about getting surgery but not sure if anyone’s had it what was it like and how successful was it jenna how did you fix your prolapse
Hey Sarah,
Well that sounds like an awful situation! If you have the opportunity to see another specialist, I would go for it. There are way more supportive options out there – especially now with COVID since you can see people virtually from other areas not as local to you and get your questions answered.
Surgery is definitely the right option for some women, but not all, so I’d get a second opinion and weigh your options based on what you think is best for your body, and your life.
Prolapse is a very individual experience but the tips I give in this blog are what I recommend all women focus on. You’d be amazed at how powerful the right alignment and breath strategies can be for helping improve your symptoms! If you can, ideally you’ll find a pelvic floor physical therapist/physiotherapist who can give you suggestions based on your body, your alignment, your breathing strategies because there are general tips, but the best approach would be to home in on your personal tendencies to get the best results.
Do you have the option to see a pelvic health physio? Or a different one if that’s the specialist you’ve already seen?
Hi Jenna,
This is all great info and makes me feel a little bit better. I am three weeks postpartum and I am pretty positive I have some degree of prolapse. I do have an appointment coming up with a physical therapist but until then I have been and know I will continue to scour the Internet for information. One thing that really freaks me out is the term “managing symptoms”. I don’t want to just manage my symptoms for the rest of my life. I want this to go away. I want there to be a cure. Can you shoot me straight? Can prolapse ever going to completely go away without surgery?
Hey Lexi,
I hear you. I like straight answers too. The honest truth is that, yes, some women are able to essentially heal their prolapse. They likely don’t have the exact same pelvic organ placement as pre-pregnancy but they no longer deal with ongoing symptoms on a daily basis.
Some symptoms may come and go throughout your cycle. But there is a chance that you can be completely asymptomatic. Especially if it’s a mild prolapse.
You’re still very early postpartum so there are lots of options beyond surgery. I’m glad you’re getting in to see a physical therapist. They’ll be able to answer your questions and give you the best options for you.
In the meantime, research has shown that meditation can be very beneficial for women with prolapse. Since you think you have it, there can be a tendency to tighten, or kegel a lot. But what your body actually needs is for you to relax and release – the more you try to kegel and “hold” things in, the more symptomatic you’ll likely be. So meditation can really help you relax and release and focus on great breathing techniques. It’s an option to try right now that can make you feel good that you’re taking some positive steps forward.
Good luck with your appointment!
Hi Jenna I feel a little bit relief have been ashamed of myself still asking how I got pop cause am just 26years and Hv not had any childbirth, am scared of settling down with a man, I really want to have my own kids , will my prolapse get worse wen am pregnant . For now am having frequent discharge and heaviness in my vaginal wall and my buttocks , and frequent urge to urinate
Hey Amos,
I hear you, it can feel very scary! But you don’t have to be ashamed of yourself. I know it’s easy to beat yourself up about this, but it is not something to feel shame over. It is very common and something that is treatable and manageable with the right support.
Have you been able to get checked out by a physical therapist or doctor? They would be able to give you the best advice for you in terms of pregnancy.
Plenty of women have healthy, comfortable pregnancies with POP so it is absolutely an option.
Hi, this was a very helpful article! I have had a vaginal partial Hysterectomy about 5 years ago and today was diagnosed with a stage 2 vaginal wall prolapse. I have been wondering if something was wrong for a few years now as sex was uncomfortable and I had to give up running as it caused a very uncomfortable heavy feeling in my vagina. I feel scared that this will be something I have to deal with forever and at 45 I feel worried about what will happen as I get older.. It seems like the “worst care” is surgery…which I would be happy to have if it would fix the issue!! I wonder if other women have has successful surgeries that have ended with no other surgeries? I sure hope so!
Hey Milo,
You are definitely not alone – however there are options to help you feel more comfortable during sex and get back into running and other activities.
The truth is that surgery can be a great option for a lot of women. Especially if they do prolapse-specific strength-training prior to and following the surgery. It doesn’t have to feel like the last resort and can be a viable, long-term option if you work on things like strength-training, alignment, optimal breathing strategies, and the like.
I hope you find a solution that works for you!
I’ve been dealing with prolapse for about a year now. I was unaware I had one because symptoms were mild and disappeared after weaning so I kept lifting my older child. I few months ago I suffered a back injury and prolapse at the same time for lifting. I went to physio and ended up getting an extremely tight pelvic floor muscle from all the kegles she told me to do which caused even more problems and made the prolapse worse. I’m switching physiotherapists now since this one also recommended I start running (what!). I found for me, yoga helps much more than kegles right now. I’ve been trying to get back into kegles but I keep suffering more symptoms. I’m not sure if I should just give them up or wait longer to start them again (it’s been 4weeks).
Hey Jenna,
It’s awful you had to go through all that frustration but I’m glad you’re looking for a new physio to help you in the future. Unfortunately they aren’t all amazing so sometimes it takes a while to find the best fit.
It’s also incredibly common for women with prolapse to have tight pelvic floors – which is why kegels aren’t always the best option. It sounds like you could use some pelvic floor release and relaxation in conjunction with full body and core strengthening (which is what is helpful for most women with prolapse).
If you haven’t already, I highly recommend you check out this video I recorded. I think you’ll find it helpful: https://jennadalton.com/insanely-good-pelvic-floor-release-stretches/
Good luck finding the right physio and I hope that video helps!
I completely understand how this can make a person think of suicide. I said think, not do.
We as women have been betrayed by doctors both male and female who are so trained to promote vaginal births that they don’t consider the horrific mental and physical torment of prolapse. If I only was told the risks.
I was told about 15 years ago I had some prolapse but it didn’t bother me. But now that I am postmenopause, I am plagued not only with prolapse, but UTIs, and the need for double hip replacement. Pessaries increase UTIs and I can’t deal
with hip replacement while I have this. I know it can happen to anyone, but I can’t help but regret not having a csection 25 years ago. And of course now with Covid, good luck getting any medical appts.
It’s awful that you’re going through this, Mi. I hope you’re able to find the support you deserve.
Have you considered seeing a therapist for mental health reasons in addition to getting physical therapy? Getting that psychological support can be so incredibly important to help navigate this issue.
Hi Jenna,
Very nicely done article, I just stumbled upon it. I had 3 large babies within 4 years and at the age of 64 suddenly had uterine prolapse. Symptoms back pain and cramping. I was shocked. Took 5 months before I saw a doctor and another 5 before I saw a urogynecologist. Kegals really made no difference, saw a specialist PT. Estrogen suppositories made a HUGE difference in the back pain, but the cramping still there. Now I have a pessary (took 4 fittings) which helps a lot but I still do not feel like my old self. Cannot exercise, went on my eliptical and immediately knew to stop. My next step is surgery which I would like to avoid, but the Kegals, pessary and estrogen are not enough. I am a very healthy person otherwise and I have a lot of living left to do. Not to mention that sex with a pessary is impossible, they say yes but NO. Taking the pessary out is TORTURE, very painful. So surgery is next…sigh. I am still working full time so it is hard to take that much time off from work.
Hey Joanie,
I hear you – there are certain exercises that might not feel great initially until you’ve built up strength and/or incorporated great breathing, engagement, and movement patterns.
Have you tried any form of strength training? Typically with my clients, I start with strength training before any form of cardio as we need to rebuild that strength – which is important even if it’s been years since you’ve had your last baby.
I’m a big advocate for strength training with prolapse. It’s not something you have to avoid. It’s something you can do with a mindful, experienced approach. You may even be able to find a physical therapist in your area that can help build a routine for you.
I hope that helps!
Per usual no support for young childless women with this condition.
Actually all the suggestions can be helpful regardless of age or whether you’ve given birth.
I am diagnosed with 3rd degree uterine prolapse, cystocele and rectocele. I have all of the symptoms you have mentioned above. When I am diagnosed with this, I feel like my life has ended. I cried alot, feel depressed n anxious. I am so hopeless so please can you tell how to deal with it.
It sounds like you’re (understandably) feeling really hopeless, sad, anxious and possibly frustrated as well. While I focused a lot on the physical side of things, the emotional and cognitive stuff is important as well. Do you have the ability to see a psychologist or therapist to help support you? Many women find this helpful ❤️
You are frequently recommending a thorough gyn exam for women who are told the can’t have a prolapse for whatever reason. My IUD strings were scratching the outside of my body during bowel movements for a year, but I was told that wasn’t possible, the strings were too short, and my cervix was right where it should be. Well, sure it was, when I was lying down with a speculum inserted. I finally started using a mirror during BMs and describing what I saw did the trick and got me a referral to urogyn. Now working my way through that process, but just because you have a thorough exam doesn’t mean it’s the right kind of exam or your particular ob/gyn is experienced in looking for prolapse. The uro/gyn surgeon agreed I had a prolapse within the first few seconds of my exam. Don’t give up, but remember you may have to change tactics to get the help you need.
Absolutely G! I actually recommend women see a pelvic health physical therapist/physiotherapist who assesses in various planes (not just laying on your back). Not all pros in the field do this (OBs are often not trained to do this, while some PTs are), but it is fortunately becoming more common as more information and awareness becomes available.
And I agree – don’t give up. It can feel frustrating and disheartening but eventually you will find the right fit, and the support you deserve!
Hi! This article was very claming to me. I’m 27, never gave birth and think I might have bladder prolapse. I think it is possible because I exercise with heavy weights, work with children (lift them up etc) and I have it in family (aunt and grandma).I will see my gynecologist tomorrow. I only hope that I will be able to find experts like pelvic floor physiotherapist here in Croatia. We are not so developted. Anyway, thank you very much for advices and all the positive and calming sentences! 🙂
Hey Marina,
I’m so glad you found this calming! I hope you’ve been able to find a physiotherapist, or someone knowledgeable about prolapse to help support you. There may even be the option to have a virtual session with someone outside your city 🙂
Treatment of severe uterine prolapse.i have this problem
Hey Negar,
Have you been able to see a pelvic health physical therapist? Or an OB knowledgeable in this area?
Thank you so so much for writing this – I was feeling pretty terrified about it but now I feel like there is hope.
You’re so welcome, Nat! I hope you find the resources and support you deserve 🙂
I have so much stress over my enterocele and rectocele that I’m in anxiety and stress and have closed my anus over it . How do I overcome this. I’m having trouble with BM and leakage. How do,I let go and relax?
Hey Tracy,
This is much more common than you would think – a lot of times a prolapse diagnosis makes you want to squeeze everything in tighter to try to “hold it in”.
A trip to a pelvic health PT and some pelvic floor relaxation exercises may help.
Have you tried these? https://youtu.be/ARXIZNanKvA
Hi all, I wanted to share some positive ways I’ve been managing my mild (didn’t seem mild to me) rectocele following my third birth. With these steps, I’m no longer obsessing over it, am experiencing fewer bulges, and am entering into a new healthier phase of life.
*PT: I’ve been seeing an excellent pelvic floor PT and actually doing the exercises as prescribed.
*Swimming: I’ve committed to swimming 4x/week to strengthen my entire body and core. It’s been making me feel good about my body, rather than depressed about the POP.
*Diet: I’m filling up on protein (to reinforce the PT and swimming) and fiber. I begin each day with chia seed pudding (super high in fiber) topped with fruit. I also drink a lot of water.
*Emsella: I had six sessions which immediately cured the leaking I was still experiencing postpartum. While it makes no claims about POP, I believe it helped.
There is a lot of despair in the comments here. There are hopefully some promising treatments coming, including lasers (Google Fotona laser) and treatments with platelet rich plasma.
Thank you so much for spreading some hope and sharing your personal experience with prolapse, Dee. There’s so much power in a sense of community and feeling like you’re not alone!
It’s awesome you’ve found some helpful approaches and you’re right, hopefully some newer technologies will create a waterfall of positive results within the next few years.
Have prolapse for about 2 years now i hame 69 do Kegel very hard to live with it and scared when i see spots of blood and get very sore
Thank you for this information. I’m 2 months postpartum and afraid may have a rectocele. I bad so much anxiety that I went to the emergency room and they said I didn’t. Then I went to the pelvic floor therapist and also said I didn’t have it but needed to work on strength. I know I sound crazy but I feel I have it, I’m seeing my OB next week. Im so scared.
Hey Laura, It can feel scary and invalidating when you feel like you have something and others are saying no. Hopefully it is truly the case that there’s nothing to worry about.
If the OB does find something, there are options and it sounds like you could work on some strengthening (and likely relaxing) of your pelvic floor regardless, so it’s good that you’re being thorough and focusing on finding solutions. Good luck!